In Part 1 of our three-part series on falls prevention technology, we reviewed the role of technology in falls prevention and discussed how you can evaluate available technologies. Part 2 focused on how to integrate technology into a comprehensive fall prevention program. Part 3 will address how to optimize your use of technology.
Most of the information in this blog derives from a Posey ® white paper1 written by Cynthia Saver and published by TIDI Products, LLC.
Optimizing Falls Prevention Technology
Integrating technology options of all types, ranging from floor mats to chair and toilet sensors, into an organization’s fall prevention program helps to enhance its effectiveness. This starts with thoughtful evaluation of potential technology to ensure it supports patient safety and fits into clinicians' workflow.
By following a few steps — such as careful patient assessment, thorough education for patients and families, regular monitoring and follow-up, and routine assessment of staff competencies — clinicians and organizations can keep staff and patients safe. These efforts will ensure that technology is effectively incorporated into care that is truly patient-centered and yields optimal outcomes.
A Quick Reminder: The Value of Falls Prevention
Falls can lead to serious injury and even death. The infographic below provides a snapshot of the frequency of inpatient falls and just some of the associated costs.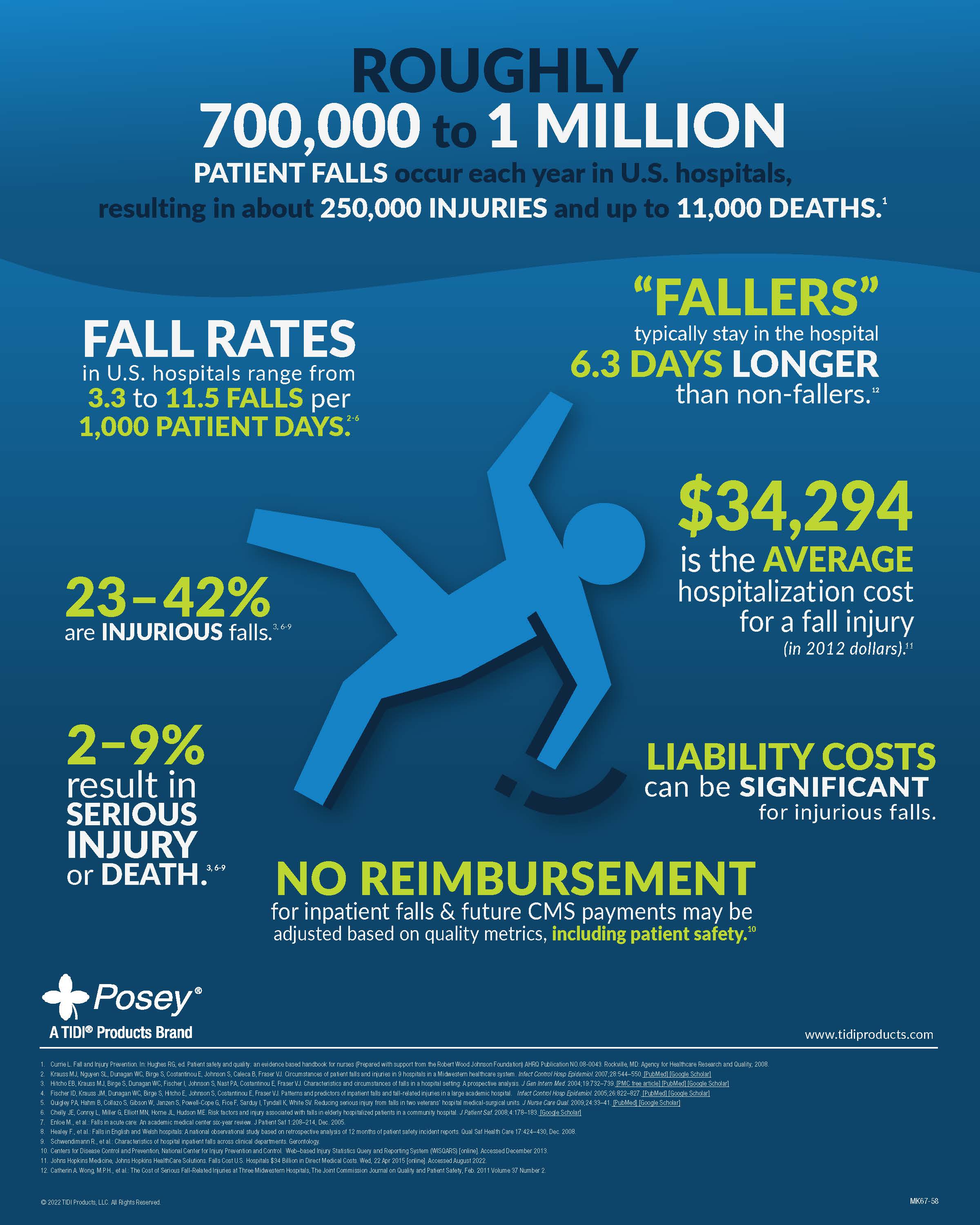
Two Trends Driving Today’s Need for Optimized Falls Prevention Technology
COVID-19 protocols. COVID-19 and its variants have made falls prevention efforts more difficult. For example, airflow requirements result in closed doors to patient rooms, limiting visual observation, and the need to add equipment such as HEPA filters increases noise levels, which contribute to distractions. In addition, nurses responding to alarms are delayed by having to don personal protective equipment before entering the room of a patient with COVID-19, and then removing that equipment before responding to an alarm from the room of another patient.
Staffing shortages. With many clinicians leaving hospital systems or long-term care settings, staff are often stretched too thin. This staff reduction, combined with prolonged work hours, may have serious consequences. For example, during the second quarter of 2020, rates of falls that caused major injury increased by 17.4% in skilled nursing facilities, according to data submitted to the Centers for Medicare and Medicaid Services.2 In addition, a report from the American Nurses Association notes that inadequate nurse-patient ratios increase fall risk, while higher RN staffing levels reduce inpatient falls.3
Optimizing Falls Prevention Technology for Hospitals
To provide caregivers greater flexibility when monitoring patients at risk of a fall, TIDI Products has developed the Posey On Cue® PRO platform. This wireless technology solution utilizes an alarm, a wireless chair sensor pad, and a wireless nurse call adapter.
Key advantages of this versatile falls prevention technology platform include:
- Optimized for ease of use, efficiency, and patient safety
- Overcomes room layout headaches via wireless monitoring
- Wireless adapter enables nurse call alerts to your station
- Tap-2-Pair™ technology establishes wireless connection with a simple tap
- Paired alarm need not be tethered to the headwall; it can be placed for easy staff access
- Large, easily visible status light on alarm confirms active monitoring
- Simple instructions for use are printed directly on each chair sensor pad to guide setup
- No new trip hazards are introduced to room environment when setting up the sensor pad
- Battery life of the single-patient wireless sensor pad is 30 days
For facilities that are not fully committed to wireless technology, the On Cue PRO platform is also compatible with traditional (wired) Posey sensors and nurse call systems.
Pilot Site Feedback
To evaluate the effectiveness of the On Cue PRO platform, a pilot was conducted on a variety of units in academic and community acute care hospitals in six states from September 2021 through March 2022, with facilities and timing staggered due to the COVID-19 pandemic. A survey was distributed to clinicians in participating hospitals to determine user satisfaction and effect on patient safety. In all, 98% of survey respondents said they would advocate using the product in their facility. Furthermore, 97% either agreed or strongly agreed that they would recommend the product (see the respondent data presented in the bar chart below).4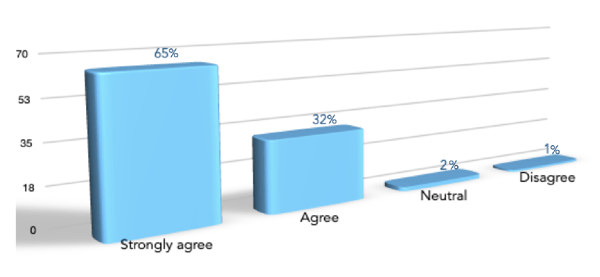 A high percentage of the respondents also agreed or strongly agreed with the following statements:
A high percentage of the respondents also agreed or strongly agreed with the following statements:
- This product improves patient safety (94%)
- The freedom to monitor patients wirelessly will improve patient care (92%)
- This product increases my flexibility to monitor the patient anywhere in the room (91%)
- The product audibly and visibly gives me confidence that the patient is being monitored safely (93%)
- This product makes my job easier (90%)
- The product is easy to troubleshoot if necessary (89%)
- Training for proper use and application was clear and helpful (98%)
- The instructions printed on the chair pad were easy to understand (96%)
- The product is easy to apply and use ― including wireless pairing (94%)
- The product works well with other products, for example, a wheelchair (93%)
Posey Education
To explore the role, evaluation, and integration of falls prevention technology more thoroughly, you can download our falls prevention technology white paper.We also encourage you to learn more about our new Posey On Cue PRO wireless technology solution for falls prevention.
1 Saver, C. Role of Technology in Falls Prevention: A Patient-centered Approach [White Paper (2022), TIDI Products, LLC].
2 Fleisher LA, Schriber M, Cardo D, Srinivasan A. Health care safety during the pandemic and beyond — building a system that ensures resilience. N Engl J Med. 2022;386(7):609-611. doi:10.1056/NEJMp2118285
3 American Nurses Association. Optimal nurse staffing to improve quality of care and patient outcomes: Executive summary. 2015.
4 Pilot survey data on file.
INFOGRAPHIC SOURCES
1 Currie L. Fall and Injury Prevention. In: Hughes RG, ed. Patient safety and quality: an evidence based handbook for nurses (Prepared with support from the Robert Wood Johnson Foundation) AHRQ Publication NO.08-0043. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
2 Krauss MJ, Nguyen SL, Dunagan WC, Birge S, Costantinou E, Johnson S, Caleca B, Fraser VJ. Circumstances of patient falls and injuries in 9 hospitals in a Midwestern healthcare system. Infect Control Hosp Epidemiol. 2007;28:544–550.[PubMed][Google Scholar]
3 Hitcho EB, Krauss MJ, Birge S, Dunagan WC, Fischer I, Johnson S, Nast PA, Costantinou E, Fraser VJ. Characteristics and circumstances of falls in a hospital setting: A prospective analysis. J Gen Intern Med. 2004;19:732–739.[PMC free article] [PubMed] [Google Scholar]
4 Fischer ID, Krauss JM, Dunagan WC, Birge S, Hitcho E, Johnson S, Costantinou E, Fraser VJ. Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital. Infect Control Hosp Epidemiol. 2005;26:822–827.[PubMed] [Google Scholar]
5 Quigley PA, Hahm B, Collazo S, Gibson W, Janzen S, Powell-Cope G, Fice F, Sarduy I, Tyndall K, White SV. Reducing serious injury from falls in two veterans’ hospital medical-surgical units. J Nurse Care Qual. 2009;24:33–41.[PubMed] [Google Scholar]
6 Chelly JE, Conroy L, Miller G, Elliott MN, Horne JL, Hudson ME. Risk factors and injury associated with falls in elderly hospitalized patients in a community hospital. J Patient Saf. 2008;4:178–183. [Google Scholar]
7 Enloe M., et al.: Falls in acute care: An academic medical center six-year review. J Patient Saf 1:208–214, Dec. 2005.
8 Healey F., et al.: Falls in English and Welsh hospitals: A national observational study based on retrospective analysis of 12 months of patient safety incident reports. Qual Saf Health Care 17:424–430, Dec. 2008.
9 Schwendimann R., et al.: Characteristics of hospital inpatient falls across clinical departments. Gerontology.
10 Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS) [online]. Accessed December 2013.
11 Johns Hopkins Medicine, Johns Hopkins HealthCare Solutions. Falls Cost U.S. Hospitals $34 Billion in Direct Medical Costs. Wed, 22 Apr 2015 [online]. Accessed August 2022.
12 Catherin A. Wong, M.P.H., et al.: The Cost of Serious Fall-Related Injuries at Three Midwestern Hospitals, The Joint Commission Journal on Quality and Patient Safety, Feb. 2011 Volume 37 Number 2.
