In Part 1 of our two-part series addressing inpatient fall rates, we review the organizational costs of inpatient falls and discuss the use of restraint-free, self-releasing technology for fall prevention. Part 2 will explore the ways in which organizations can augment their multifactorial fall prevention protocols by implementing this type of technology.
The information in this blog derives from a Posey® white paper1 written by Julie Nyhus and published by TIDI Products, LLC.
“I don’t know how much the Posey HeadStart Notification Sensor Chair Belts cost, but I’m sure it’s not as costly as treating a fall. That’s why getting leadership on board with this product was so easy.”
― Emily Hess, RN, BSN, Clinical Educator at Aspirus Wausau Hospital in Wausau, Wisconsin
An Ongoing Problem: Inpatient Falls
Inpatient falls remain one of the most vexing patient-safety problems facing healthcare leadership, impacting clinical and financial outcomes. By applying multifactorial fall prevention strategies, organizations have lowered fall rates in the past. Yet, falls and injuries from falls continue to devastate patients and their families, indicating that multifactorial fall prevention protocols alone are not enough.
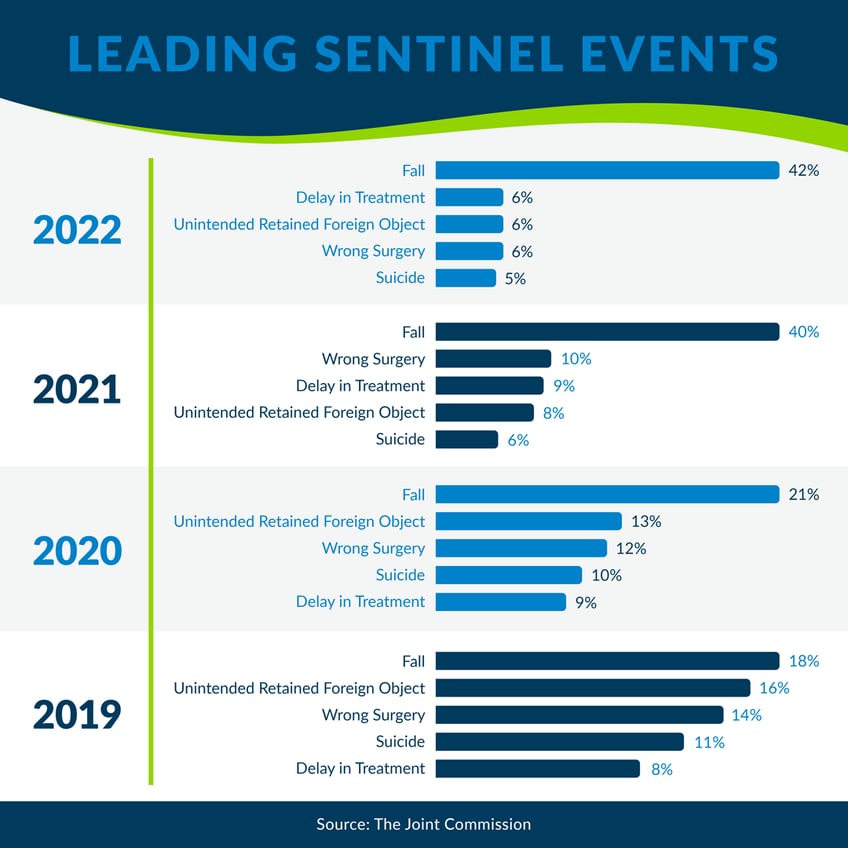
In its Sentinel Event Data 2022 Annual Review, The Joint Commission (TJC) identified falls as the leading sentinel event for the fourth year in a row.
The Organizational Costs of Inpatient Falls
Healthcare organizations bear the cost of treating fall-related patient injuries. This organizational cost is twofold: (1) the expense of treating patient injuries related to falls and (2) the cost of creating and implementing organizational systems to prevent falls and injuries related to falls.
The annual cost of treating fall-related injuries averages $14,056 per patient and can add up to seven additional hospital days. The estimated annual cost of treating serious injuries related to inpatient falls in the U.S. is $50 billion.2
Meanwhile, even though organizations expect to incur costs to implement multifactorial strategies to reduce their fall rates, these interventions are costly. One systematic review reported that the cost to design and implement multifactorial fall interventions ranges from $4,300 to $120,000.3
From National Directives to Multifactorial Interventions
Efforts to prevent inpatient falls and injuries gained momentum nationwide after TJC’s 2015 Sentinel Alert 55 published that falls with serious injuries were consistently reported among the top ten sentinel events.4
To address that “sustained reduction [of falls] has proven elusive,” TJC recommended several evidence-based strategies for fall prevention and reduction, allowing healthcare leaders to decide which ones are best suited for their organization’s needs.4
In response, many organizations created new fall prevention protocols and guidelines by replacing simple fall risk score calculations with multidisciplinary approaches that included several TJC-recommended actions.5
The most successful multifactorial fall prevention programs implemented TJC strategies such as:
• Improving fall risk assessment processes
• Adding visual cues to alert staff of high-risk patients
• Addressing staff communication regarding fall risk status
• Ensuring adherence with protocols and safety practices, such as focusing on safety transfers while toileting
• Improving education of patients and all staff levels
• Correcting deficiencies in the physical environment, such as use of alarm mats and low beds
This laborious process resulted in numerous multifactorial fall prevention approaches, each unique to its own organizational system. Yet, even with multifactorial fall prevention in place, inpatient falls and injuries are ongoing, complex, and costly. Are there cost-effective steps healthcare leaders can take to boost the multifactorial fall prevention protocols they’ve already initiated?
Non-Restraint Fall Prevention Tools
Over recent years several technology-based fall prevention applications have emerged to prevent, detect, and monitor falls, including non-restraint, self-releasing technology designed to allow patients to turn, sit up, shift, and move in beds and chairs while providing the opportunity for them to self-release.
According to the Centers for Medicare & Medicaid Services (CMS), self-releasing alarm belts are classified as fall prevention tools, not restraints.6

If a patient can “easily remove” a device, the device would not be considered a restraint. “Easily remove” means the manual method, device, material, or equipment can be removed intentionally by the patient in the same manner as it was applied by staff.6
For organizations who have mastered the proper application, teaching, and documentation of these devices, non-restraint, self-releasing technology is quickly becoming a commonly used fall prevention tool. This technology provides the earliest possible notification that a patient is at immediate risk of exiting a chair or bed, while simultaneously providing staff additional time to respond — all without restraints.
Merging Protocol with Technology
Unit leaders at the Center for Rehabilitation at Wilmington Hospital reported that the use of “self-releasing alarm belts” for qualifying patients was their “most significant and most effective decision” when seeking to lower their center’s overall fall rate.7
In addition to revamping their multifactorial approach — everything from implementing the Morse Fall Risk Assessment Tool to creating new policies on post-fall responses — Wilmington Hospital noted that using self-releasing alarm belts allowed “staff additional time to prevent a fall.”7

Yale New Haven Hospital trialed a hook-and-loop alarm belt for use alongside their multilayered fall prevention initiatives. According to Yale New Haven Hospital leaders, “The value of the belt is that it doesn’t restrain patients.” They found that the product allowed patients to remove the belt themselves, serving as a reminder rather than a physical restraint.8
Learn More Now!
To learn more about the costs associated with inpatient falls and injuries, the history of fall prevention, and how to bolster fall prevention initiatives using restraint-free, self-releasing technology such as Posey HeadStart Notification Sensors, download our white paper here.
And be sure to visit the Posey HeadStart Chair and Bed Sensors webpage today!
SOURCES
1 Nyhus, J. Inpatient Fall Rates Persist: Using Restraint-free Technology To Augment Fall Prevention Protocols [White Paper (2023), TIDI Products, LLC].
2 Kartiko S, Jeremitsky E, Cripps MW, Konderwicz I, Jarosz E, Minshall CT. Fall prevention initiative: A fall screening and intervention pilot study on the ambulatory setting. J Trauma Acute Care Surg. 2020;88(1):101-105. doi:10.1097/TA.0000000000002514
3 Alipour V, Azami-Aghdash S, Rezapour A, et al. Cost-Effectiveness of multifactorial interventions in preventing falls among elderly population: A systematic review. Bull Emerg Trauma. 2021;9(4):159-168. doi:10.30476/BEAT.2021.84375.1068
4 JointCommission.org. Preventing falls and fall-related injuries in health care facilities. Sentinel Event Alert 2015:1-5. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_55_falls_4_26_16.pdf
5 Turner K, Staggs V, Potter C, Cramer E, Shorr R, Mion LC. Fall prevention implementation strategies in use at 60 United States hospitals: a descriptive study. BMJ Qual Saf. 2020;29(12):1000-1007. doi:10.1136/bmjqs-2019-010642
6 Centers for Medicare and Medicaid Service State Operations Manual – Appendix A, Rev. 200, 02/21/20. Accessed November 8, 2021. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_a_hospitals.pdf
7 Alderson FE, Boivin J. Self-releasing alarm belts: It takes two. American Nurse Today. 2017;12(3):25-26.
8 Wicker D, Boivin J. Hook-and-loop alarm belt: A vital component in a fall-prevention toolkit. American Nurse Today. 2017;12(1):26-27.
